Did you know that about 48% of women who are pregnant for the first time will have signs of incontinence by week 30 of their pregnancy. In women who have given birth before this rate increases to 67%. That is half, half of women who have never given birth before suffer from incontinence…that number shocked me. It shocked me not because of the fact that it happens (I mean you are growing a human being after all that is pressing down on your bladder and pelvic floor), but what shocked me was how little it seems to be spoken about, especially if it really is this common.
Incontinence can present in many ways but the most common way is urinary incontinence, which is the involuntary loss of urine. Incontinence can also refer to flatal incontinence which is the involuntary release of gas or fecal incontinence which is the involuntary loss of feces. Both of these are less common than urinary but you can see how fecal incontinence especially can be devastating to a woman’s quality of life and self-esteem.

Because urinary incontinence is much more common we will focus our discussion on that, however know that some of the recommendations that follow will apply to other forms of incontinence as well.
There are two main forms of urinary incontinence including stress and urge urinary incontinence. Stress urinary incontinence is leakage occurring when the pressure on the bladder increases and exceeds the closing pressure of the urethra (the tube connecting the bladder to the outside of the body). This often occurs when one is exerting themselves is some way like sneezing, coughing, laughing, or exercising (running, box jumps, other high intensity movements). Urge urinary incontinence occurs when their is involuntary leakage associated with urgency (the need to use the bathroom and when they can’t make it time they leak urine as a result). In this situation the urgency can be triggered by a variety of factors like pulling down your pants, putting your key in the door when arriving at home or hearing running water. Toilet mapping is also a common behaviour for those suffering from urge urinary incontinence. This is a behaviour in which an individual located the nearest bathroom (no matter where they are) before they do anything else just in case they need it. These two types of incontinence can also present together and when they do it is called mixed urinary incontinence.
Some other forms of incontinence you may hear about but are much less common include; postural urinary incontinence (loss of urine associated with a change in body position), nocturnal enuresis (bed wetting), continuous urinary incontinence, insensible urinary incontinence (loss of urine that happens unconsciously) or coital incontinence (loss of urine during sex).
There are a number of risk factors associated with incontinence (yes pregnancy and birth is only one of them). These other risk factors include; aging, smoking, family history (genetics), a BMI of 30 or higher, menopause, neurological diseases, diabetes, the number of times one has given birth (parity) and some gynecological surgeries.

So we know that incontinence is prevalent in moms-to-be and postpartum but it’s not commonly talked about nor do many women seek treatment for it. This is often because they are embarrassed to do so or they assume that it’s common so they just have to live with it. But incontinence can affect your life in many ways and it’s important that you know that you do not have to just live with it. Commonly, incontinence can affect you emotionally, be a barrier to fitness progress, and hold you back from fully participating in activities you love. I want you to know although incontinence is common,it is not something that you just have to live with.
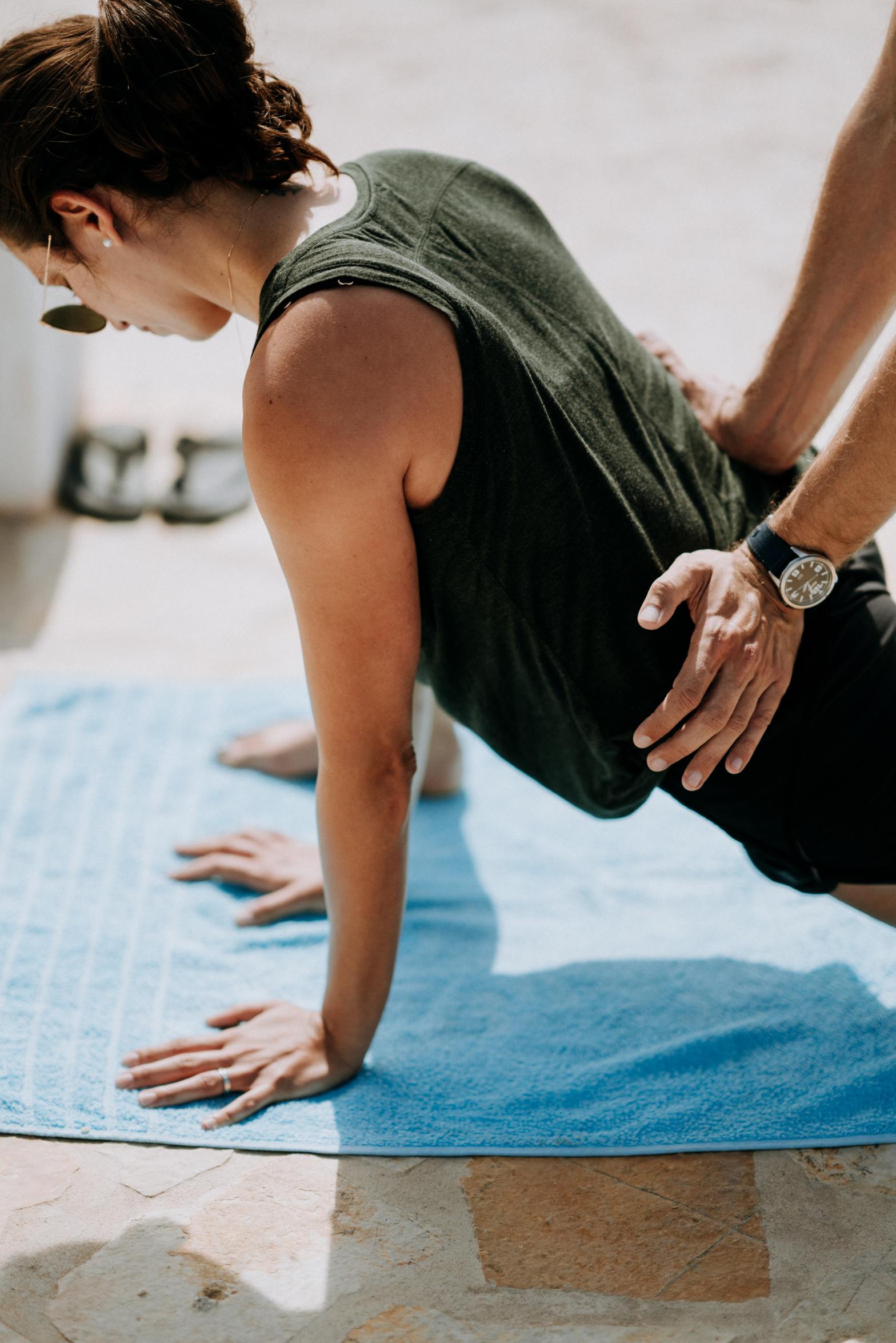
The most common treatment option for incontinence is care provided by a pelvic health physiotherapist. They will perform a clinical exam in which they will assess areas including but not limited to the hips, lower back and pelvic floor in order to identify what may be contributing to the incontinence. Some, but not all pelvic health physiotherapists will perform an internal exam as part of their assessment. Be sure that if your practitioner is performing an internal exam that you ask any questions and are comfortable with the procedure. They will likely explain the procedure to you in detail before, but if you have any questions please be sure to voice them. Once the physiotherapist knows what the cause of your incontinence is they will work with you to build a treatment plan around it that may include prescribed strengthening or relaxation exercises or behavioural interventions. Do your best to follow their prescription as closely as possible. If you are working with others individuals on your health and fitness journey like a trainer, coach or exercise physiologist they may ask to see the plan your physiotherapist has developed. Try your best to share it with them, as they are not asking to invade your privacy, but they instead want to ensure that what you are doing in your training is working with the physiotherapists prescription and not against it.
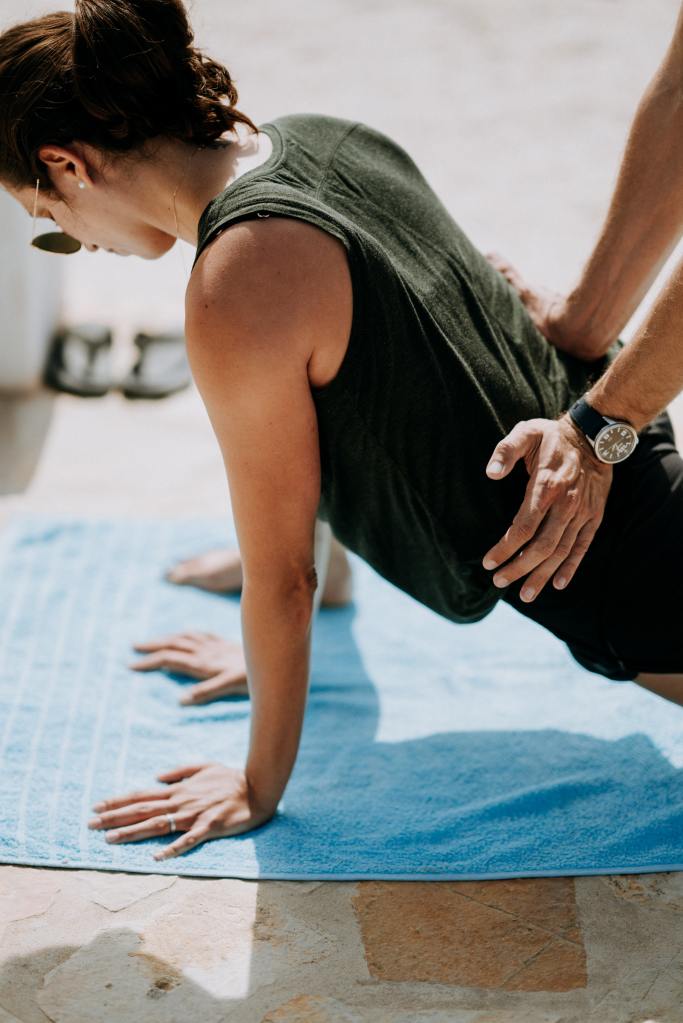
If you are experiencing incontinence when training be sure to speak to your trainer about it. Exercises can always be modified in order to accommodate while you are working on your treatment plan with your physiotherapist. Using the Connection Breath may also be helpful during your training. To learn more about the connection breath and how to perform it you can check out the post on pelvic floor health here. This breathing technique can help you tune in and feel how your breathing affects your pelvic floor and is a nice simple add on to a warmup routine. You can also share the exercises prescribed by your physiotherapist and your trainer can help guide you through those exercises as well. Always keep constant and open communication with your trainer about how you feel when you perform certain movements or use certain weights. If something is not working your trainer will work with you to adjust your program as you are addressing your incontinence.
Although incontinence is common among late pregnancy and postpartum women it is not something that you just have to live with after you’ve had a baby. Advocate for yourself, speak up and ask questions. When in doubt look for a pelvic health physiotherapist and work in conjunction with them and a trainer to get the best experience. Incontinence is not something that you have to experience for the rest of your life or let it impact your life in any way. If you have any questions please reach out and I would love to help guide you in any way possible on your journey to health and wellness. Until next week!